James’ Journey
- Britt Nicole

- Aug 4, 2019
- 14 min read
Updated: Jun 29, 2020
James Robert Joyner was born on July 15, 2018 at 15:07 via C-section at exactly 32 weeks gestational age due to complications during pregnancy. James spent four weeks in the NICU at Anne Arundel Medical Center where he was delivered. He was born breathing on his own which was a miracle in itself. While in the NICU, James had to learn how to eat on his own and how to maintain his body temperature. Those four weeks were long but on August 11, 2018, we finally got to bring James home.
On September 6, 2018, we took James to the pediatrician because he had been inconsolable for about two and a half days and we knew something was wrong. His pediatrician noticed that his fontanelles (soft spots) were bulging and his head circumference was larger than expected so he sent us to our local emergency department at Peninsula Regional Medical Center. While we were there, the doctors ran tests and took a CAT scan that revealed that James had hydrocephalus, which is a build-up of fluid in the cavities deep within the brain. The doctor explained that James would most likely need surgery to place a shunt into his brain to help drain the fluid and that we would need to be transferred to Johns Hopkins Children’s Center in Baltimore, MD. We got transported that same evening by ambulance and arrived at Hopkins later that night. When we arrived, James was admitted into the NICU (Neonatal Intensive Care Unit) where doctors and neurosurgeons met with us to discuss the plans for James. They told us he would be getting an MRI sometime overnight so they could get a better look at his brain and the fluid. They explained that the CAT scan that was taken at PRMC was unusual to them so they needed to get a better visual. Usually with hydrocephalus, there are only two pockets in the brain (the left and right ventricles), where the fluid builds up but with James, it showed that he had multiple other pockets of fluid throughout the brain, which only left them to wonder why he had fluid in other places. They reasoned that they needed to act quickly because his vitals started to look unstable. There was starting to be nowhere for all of the fluid to go and it was putting too much pressure on his brain.
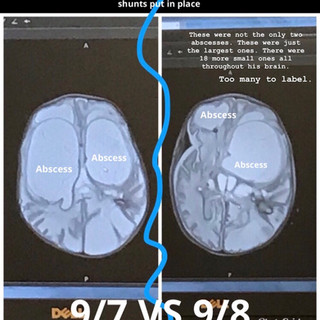
Early the next morning, James had surgery to place two shunts into his brain to help drain the built up fluid but when they went to place the shunt, they noticed that the fluid was more glue-like (puss) than fluid-like, indicating that James actually had an infection in his brain. The multiple “pockets” of fluid throughout his brain were actually abscesses, which the MRI confirmed. He had multiple abscesses all throughout his brain, in both hemispheres, front and back. His neurosurgeon, Dr. Alan R Cohen, the director of Pediatric Neuro-surgery, told us that this was an extremely rare and very serious infection in our son’s brain.
James was then admitted to the PICU (Pediatric Intensive Care Unit) after his surgery was successfully completed. The doctors immediately started James on a wide variety of IV antibiotics while they sent a culture of the fluid to the lab to determine exactly what bacteria was growing. They placed one shunt into each ventricle to drain the fluid and to relieve some of the pressure off of his brain and relieve some of the pain he had been feeling. Usually when they place a shunt into the brain, they would allow the shunt to drain the fluid back into the body at another location, but since James had an infection, they had each shunt drain into a bag, one on each side of his crib. The puss from the abscesses is what was causing a block in the ventricles causing the fluid to build up and not drain back into the body properly. The fluid built up in his brain is cerebral spinal fluid. Each day they would check his CSF (cerebral spinal fluid) to see if any new bacteria was growing and make sure his ventricles were draining properly.
The next day after James’ first brain procedure, they narrowed down the bacteria to Enterobacter Cloacae. Once they knew what exact bacteria it was, they could narrow down his antibiotics to just one specific one that targets Enterobacter Cloacae and take him off of all other antibiotics. They estimated James to have to be on IV antibiotics for 4-6 weeks, which later changed to an estimated 6-8 weeks. Not long after, James got a PICC line (Peripherally Inserted Central Catheter) inserted into his leg. A PICC line is basically a long-term IV used for long-term antibiotics, medications, nutrition, and for blood draws.
Enterobacter Cloacae is a bacteria that lives in your gut. The doctors have no idea how it got to his brain, when it got there, or where he got it from. There was no indication that the bacteria was ever in his blood but they say it’s possible that it was at one point. They explained that Enterobacter Cloacae is a very serious bacteria and a very rapidly growing bacteria as well so it’s possible, judging by the severity of James’ infection, that he may not have had his infection for too long before we brought him in but long enough to be as severe as it was. James showed no signs or symptoms of a brain infection or even being ill. He simply just cried in pain for a few days until we took him to the pediatrician, who then noticed it was his bulging fontanelles (soft spots) that were causing him pain. He had been having massive headaches and possible neck pains for days and no one would’ve ever known.
On September 9, 2018, two days after James’ first brain procedure, the doctors went back in to adjust one of the shunts as they noticed on a follow up MRI that the shunt to one of the ventricles didn’t penetrate into the ventricle, rather bounced off the aimed ventricle and penetrated the opposite one. They had to go in and use a “harder” tool to make sure the shunt penetrated into the abscess, as they discovered that this abscess was harder than what they anticipated. Later, it was shown that the procedure worked beautifully as the drains were both working properly and draining out the puss and fluid as they should. They continued to check his CSF that continued to drain into the bags. They continued to tell us each day that no new bacteria had been growing which was always good news!
On September 14, 2018, we had a family meeting with James’ whole team of doctors to discuss his course of treatment and the severe infection in his brain. The doctors explained that they didn’t know much but he would most likely have some disabilities because at this point you could already notice some brain damage on his MRI. They gave us all the possible outcomes and we discussed furthering his treatment with the shunts and IV antibiotics.
We eventually got to hold James after a week of being at Hopkins. The doctors always had him stay lying flat so his drains would stay level and drain properly but then we compromised with the doctors and were able to clamp off his drains and hold him for about 30 mins every few hours.
Eventually, there was nothing left to drain out, so he got his drains removed on September 19, 2018. A few days later on September 22, 2018 James got moved out of Intensive Care and onto the Pediatric Care and Clinical Research Unit. The doctors felt as if his vitals were stable enough that he didn’t need to be in Intensive Care anymore. This was also good news!
James was doing well but he had something called neuro-irritability that was really starting to show. He would get extremely agitated, vomit a few times a day, and get over stimulated easily. The doctors recommended a nerve medicationfor him to help with the irritability. They explained that the damaged brain cells were most likely trying to recover causing him to become irritable. They also explained that the meninges in his brain also have pain receptors and were damaged so it was possible they were sending signals causing him pain.
James also started reflux medication as well to try to help with the vomiting. When James was in the PICU he didn’t get to eat for a few days because of his brain procedures. When he finally did get to eat, we started out slowly. He remembered how to suck and eat but it was too difficult for him to put all the steps together; suck, breathe, and swallow. During the time James was in the PICU, he would’ve just been born if you went by his adjusted age (since he was born 8 weeks early). During this time, at his adjusted age, would’ve been the time when an infant learned how to eat and since he was not eating during this period of time, he had forgotten how to eat. James worked with a bottle for ten minutes on some feeds to start practicing eating again.
Within the next few weeks James got transferred to Kennedy Krieger Institute in Baltimore, MD for rehabilitationon October 4, 2018. James had occupational therapy and recreational therapy to work on keeping his arms and legs moving and work on his development. He also had a speech pathologist who worked with him on learning how to eat again. While at KKI, on October 22, 2018, James got a follow up MRI which indicated that the infection in his brain was completely gone, but we also got news that he had little to no healthy brain tissue left. The infection had destroyed his brain. The very next day, we had a family meeting with his doctors and specialists where they revealed these results and explained to us that due to the damage done to James’ brain that he would live his life with severe deficits and disabilities and wouldn’t be able to do much on his own, if at all. We were discharged later that week on October 27, 2018 to head home from Baltimore because medically there was no reason for James to be under their care anymore since the infection in his brain was gone.
We were devastated by this news but also were so excited that after spending about two months in Baltimore that we were finally able to take our sweet babyboy home with us! We knew we had a difficult road ahead of us but we’d do anything to ensure that our little boy would have the best life possible. We collected our thoughts, all of James’ things, all of our things, his medications, and equipment and we headed home with our sweet little one. He came home on an NG tube in his nose still because he was still in the process of learning how to eat. We had planned on continuing his therapy at home.
Unfortunately, we didn’t stay home for long. On October 31, 2018 we took James for a follow up appointment with his neurologist at Johns Hopkins. The neurologist looked at James’ head and became concerned and decided to admit us. The fluid in James’ head was increasing and you could start to physically see it. He had bubbles of fluid starting to poke out wherever they could. We spent the next few days at Hopkins. They ordered another MRI to get a better look and they decided that the fluid had increased a bit but was also spreading out throughout the brain so they couldn’t tell if it had increased a significant amount. They explained that the fluid within his head was shifting to other places and that makes it difficult to tell if there really was more fluid or if it was just moving throughout the brain. Regardless, James had recently been having a few crying spells where he’d scream in pain for a few hours and wouldn’t stop, which he had done the previous night before his follow up appointment. We discussed with doctors and worked with his palliative care team to come up with pain medications that would work well for James at times when he was feeling pain or discomfort. We were discharged home a few days later on November 3, 2018 once James was all checked out and we found a good pain regimen for at home care.
On November 7, 2018, we took James back to Johns Hopkins for a follow up with his Infectious Disease doctors. They just wanted to discuss the infection that he had, made sure we understood the infection and answer any and all questions that we would have. They still couldn’t tell us much of what we didn’t already know but did confirm again that the infection was gone.
Unfortunately, a few days later I had noticed that James had been sleeping quite a lot; pretty much all day long. So the next day when I noticed he had been sleeping all day again I decided to call the on call doctor at Johns Hopkins and they asked if we could bring him in to get evaluated. On that same day, November 10, 2018, we took our boy back to Hopkins where he got admitted yet again. They took another MRI to see what was going on in that head of his. They sent his images all throughout the hospital to different teams of doctors to look at to see if anyone could come up with a solution or any type of fix for all that was going on in our little boy’s brain. After getting admitted, they transferred us from the emergency department up to the Pediatric Unit where James’ neurosurgeon and team of doctors met with me early the next morning, November 11, 2018. They simply told us that there was nothing more they could do for him. The neurosurgeon explained that there were too many individual pockets of fluid throughout James’ brain that a shunt wouldn’t work and that his ventricles were so damaged that James would continue to make fluid but not reabsorb it like your body is supposed to… causing the fluid to continuously build up and continuously put pressure on his brain. The neurosurgeon did explain that we could always have surgery as an option… it would not help James, it would only make us feel better. He explained that anything else done would do more harm to James than benefit him. He simply said that no matter how many surgeries he could attempt that the outcome would eventually be the same: that we would lose our boy. They suggested doing what we could to make him as comfortable as possible. No words any parent ever wants to hear. Our sweet boy looked just like any other baby, but he was sick. You couldn’t tell from the outside because he was always so active and smiling. He sure was a little warrior and an inspiration to all of us. Of course the doctors were always so impressed when they evaluated him just because of how well he always looked but they all knew that there was nothing more they could for him besides keep his pain controlled and keep him as comfortable as possible. We spent the rest of the week at Johns Hopkins working with his palliative care team to come up with the best pain regimen that we could for James. We adjusted his medications, added mediations, and took away medications until we found a regimen that worked best for our baby. The doctors wanted to make sure James had one full good day and one good night with his pain controlled and him being comfortable before sending us home. On November 14, 2018, we were discharged home from Johns Hopkins with pain medications and an appointment set up for our son to be put on Pediatric Hospice Care. The next day after being home, Coastal Hospice workers came by the house to discuss plans with us and to meet our sweet James.
For the next few weeks, we spent our days like we always have, snuggled up with James all day long and giving him all the love we possibly could. On November 22, 2018 we spent James first Thanksgiving with all of our family. He was surrounded by love all day long, just like any other day. We were so thankful to have gotten to spend his first and only Thanksgiving with him.
A few days later, James’ body was starting to show signs of shutting down. He was no longer able to tolerate his tube feedings anymore. He would vomit, get fussy from tummy aches, and his stomach would remain full all day off of just one feeding. His body could no longer digest or handle his food anymore so we decided to think more about his comfort than his nutritional needs. We stopped his tube feedings and started him on Pedialyte throughout the day just to keep him hydrated. After about a week, we stopped the Pedialyte as well, and he was only getting medications through his tube and that was it. Near the end of November, first few days of December is when we really started to notice James declining. He would lose control of his eyes, just stare blankly like he wasn’t really “there” anymore, not move much, not much output in his diaper, and his body became stiff most days. On the evening of December 13, 2018 we thought it was James’ time. There were a few times before this day when James was not looking well and we were unsure if he’d make it through the day. On the night of the 13th, James was only breathing about 1 breath every 3 minutes. We all thought he couldn’t survive for long breathing like this. But he did. The very next morning on December 14, 2018 James went into cardiac arrest while mommy was holding him while sitting on the couch watching a movie. It was 11:27 am when he stopped breathing. We were devastated and heartbroken. His hospice nurse came and evaluated him. When calling time of the death, the hospice nurse must listen to his heart for two minutes. After listening to James, about 30-40 minutes later after his arrest, she explained to us that he did not have a heartbeat for the first minute of her listening but for the second minute his heart started right back up into normal rhythm… MIRACLE! No one knows how or why and no one can explain it. Our baby just wasn’t ready yet.
The next day, December 15, 2018 our sweet baby James was exactly 5 months old. He spent all day like he usually did, cuddling with family and being loved. Around 8:45 pm that night, James stopped breathing again for about five minutes while in his daddy’s arms. We watched James closely for the rest of the night. He stopped breathing, took 1 breath every 3 minutes, started to breathe regular again, stopped breathing again for about 25 minutes yet still had a heartbeat, breathe normally again, breathe once every 5 minutes and so on. We would periodically check for a heartbeat. His heart would become very fast, then slow down, then beat normally, then it would stop beating for a seconds then start back up again and this crazy cycle would repeat. Every night before we go to bed, daddy ALWAYS gave James a nice, snuggly hug as we’re going to bed. Whether James stays locked in his daddy’s arms or if the hug is just for a few minutes and then daddy laid him back down in between us, no matter what, James would always get that hug every night as we’re going to bed. So as we’re lying in bed with our babyboy, his daddy looks over at him and says “what’s wrong bud? You just need a hug? You want to cuddle?” and he grabbed James, cuddled him up to him like he always does and then all of a sudden, he feels James’ whole body relax. That was it. He set James back in between us, got the stethoscope and listened, no heartbeat. It was now 1 am on Sunday, December 16, 2018. We spent the next few hours allowing family to come say their goodbyes to our sweet boy as we also said our goodbyes as well. We took the last 30 minutes with him toourselves to have our last few cuddles and last few words with our son. The funeral home showed up to the house around 3:30 am to take our son away. I think that was one of the hardest parts... was letting him go and giving him away.
On December 20, 2018 was James’ funeral. It was a beautiful service with many people who surrounded us and showed a great outpouring of love for our son. We decided to have James cremated so no matter what, we would always have a piece of James with us no matter where we are.
We will be forever grateful for the five months we got to spend with our beautiful son. It is because of not only our own efforts as his parents but because of multiple people’s efforts that we got to spend this time with our son.
We will always be thankful and appreciative for our family who stood by us and our son and supported us throughout this whole journey. We will always be thankful and appreciative forthe doctors, nurses, and surgeons at Johns Hopkins Children’s Center for taking care of our son and our family as we spent much of our time there. We believe these doctors, nurses, and surgeons did the best that they could possibly do to the best of their abilities to care for our son. We will always thank and appreciate the doctors, nurses, and therapists at Kennedy Krieger Institute for taking care of our son and our family while he was in their care. We will always be thankful and appreciative for The Ronald McDonald House Charities of Baltimore for giving us a place to stay that felt like a home away from home while we were going through this with our son and were hours away from our real home. We will always be thankful and appreciative for every single person who reached out to us, made our family dinner, sent cards, made donations, sent care packages, sent flowers, checked up on us, messaged or called us. We will always be thankful for every person that followed James’ story every step of the way.
































































































Comments